Excellent Patience Experience at Radnor

RADNOR, Pa. – Each quarter, GSPP Rehabilitation’s Patient Experience Leadership team recognizes excellent Patient Experience in the areas of Innovation, Service and Teamwork. Award recipients are chosen based on their scores and input from the Patient Experience Leadership Team.
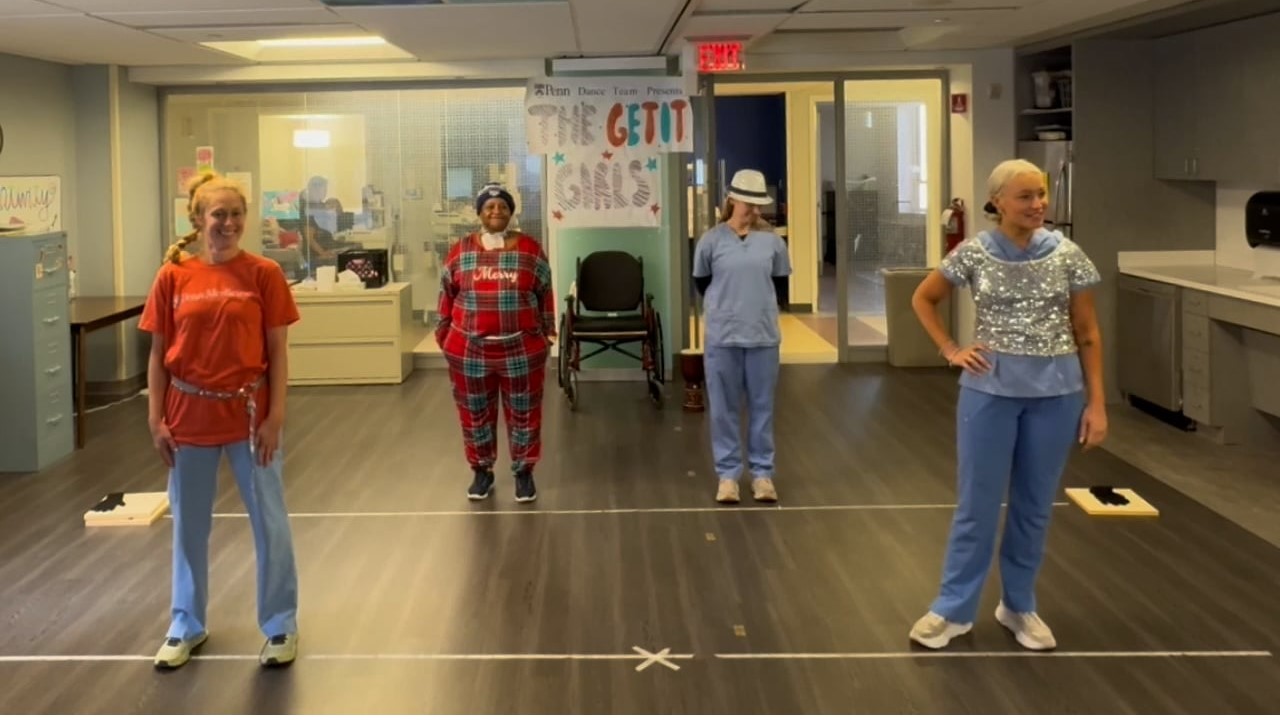
The Patient Experience Leadership Team is pleased to share Penn Medicine | Good Shepherd Rehabilitation Outpatient Therapy in Radnor is the recipient of this quarter’s Patient Experience Award for Teamwork. This is one of three patient Experience Awards that celebrates and recognizes our continuous dedication to improving the patient experience.
Members of the Radnor leadership team say the secret to their success lies in collaboration and focus on the patient.
“Our focus on the patient experience unifies our entire team, from the front to back,” said Regional Manager Sean Loughlin. “We are a ‘care team’ who strives to exceed our patients’ expectations every day. We involve them in developing their care plans, which makes them an essential member of the team. This singular focus results in extraordinary teamwork.”
Lead Therapist Jimmy Newton agrees.
“Radnor is special because it’s like a family of highly skilled providers who show up every day to help and support one another which allows each of us to provide the highest level of care to our patients and the community,” Jimmy said.
Congratulations, Radnor team!